As companies continue to scrutinize healthcare partners’ effectiveness, some employers are taking cost savings into their own hands. One of the ways they’re doing it is through more direct relationships with the provider community.
The idea is familiar to many executive teams: Just as you negotiate contracts for products and services for your company, the same opportunity exists between employers and providers. Direct arrangements with providers are implemented to lower overall costs by improving pricing transparency and eliminating “middle-men” entities, which in today’s environment can be significant barriers for better managing healthcare.
In this article, we’ll review how direct contracting works for employers, best practices for implementation and future predictions for the trend.
Rather than pay premiums to traditional health insurance companies to accept unknown carrier network pricing, employers contract directly with provider facilities to be their preferred points of service for employees’ healthcare needs. Many times, employers prioritize contracts for highest-cost and most frequent healthcare needs. The practice can be considered an extension of narrow networks, which make a smaller number of high-value providers available to employees.
Different contract types existing within direct contracting, from fee for service, risk-based (using capitation or other global payment methods), service level agreements and in some cases, medical tourism. One popular example of direct contracting is Walmart’s arrangement with the Cleveland Clinic for cardiac surgery. The retailer also partners with Johns Hopkins Hospital in Baltimore for joint replacement surgery and the Mayo Clinic for transplants and cancer care.
While these are enterprise-level programs, it’s important to note that the same opportunities can exist on the local level.
Direct contracting works best when:
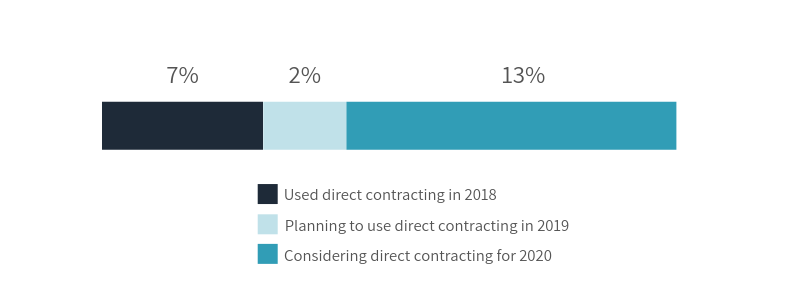
According to a national survey, the prevalence of employers using direct contracting could triple by 2020.
Businesses of all sizes can benefit from a direct contracting arrangement because it opens a direct discussion about cost and quality that are not traditionally available. As a result, companies can see significant savings from successful direct contracts.
Direct contracting also:
While direct contracting is a feasible solution for most companies, it’s critical to have the right partners on hand. Contracts must make financial sense for all parties and companies must be prepared to coordinate all of the moving pieces.
To help, look for a partner with:
An additional element to consider: Effective steerage to low-cost, high-quality facilities can many times achieve similar results to a direct contract.
It is likely we will continue to see an increase of direct contracts and narrow network options that return networks back to serving their original purpose as a defined set of preferred providers based on quality and cost. Successful direct contracting can help employers successfully navigate this shift.
Direct contracting is just one way companies are saving on healthcare. Download our latest report: 3 Strategies from Companies Spending 22% Less on Healthcare to learn more.